Why Understanding Eosinophilic Esophagitis Treatment Is Critical for Your Health
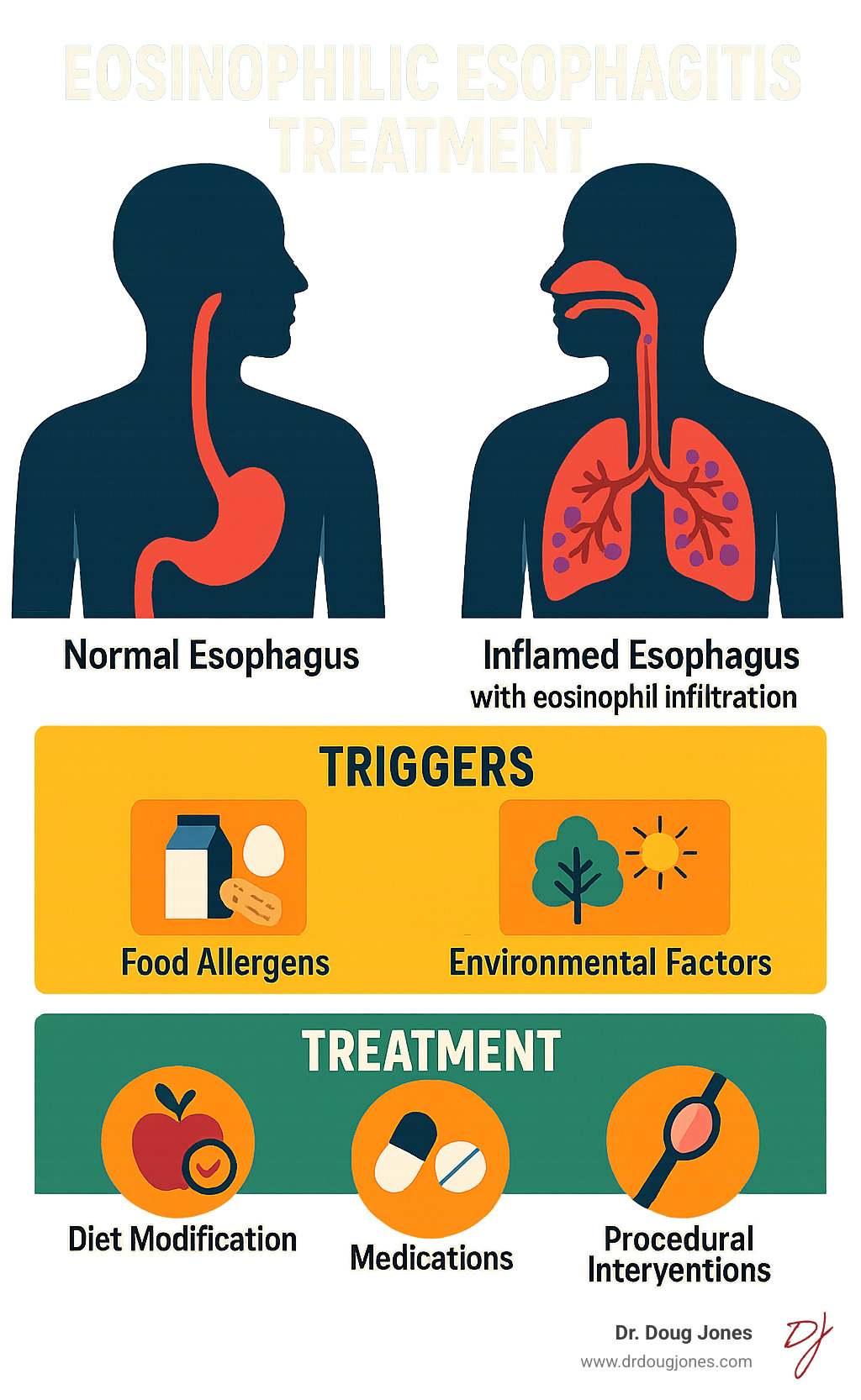
If you struggle with difficulty swallowing, chest pain, or food getting stuck, you might have eosinophilic esophagitis (EoE). This chronic immune condition causes white blood cells (eosinophils) to build up in your esophagus, leading to inflammation and serious complications. Eosinophilic esophagitis treatment is critical for managing symptoms and preventing long-term damage.
EoE symptoms vary by age. Infants may refuse to eat, children often have abdominal pain and vomiting, while teens and adults typically experience difficulty swallowing (dysphagia), sometimes leading to food impactions that require emergency care.
Without proper treatment, EoE can cause permanent scarring and narrowing of the esophagus. Research shows the risk of this narrowing (a stricture) doubles for every 10 years a patient ages, making early intervention crucial.
Effective treatment involves three main pillars:
- Dietary Management: Identifying and eliminating trigger foods.
- Medications: Using therapies like proton pump inhibitors, topical corticosteroids, or biologics to reduce inflammation.
- Procedural Interventions: Performing esophageal dilation to widen the esophagus when necessary. Repeated dilations are not ideal and the better approach is to prevent this in the first place.
As Dr. Doug Jones, a board-certified immunologist, I specialize in helping patients steer their EoE treatment journey. My integrative approach focuses on addressing root causes, not just symptoms, through a personalized, multidisciplinary plan that empowers you to take control of your health.
The Core Pillars of Eosinophilic Esophagitis Treatment
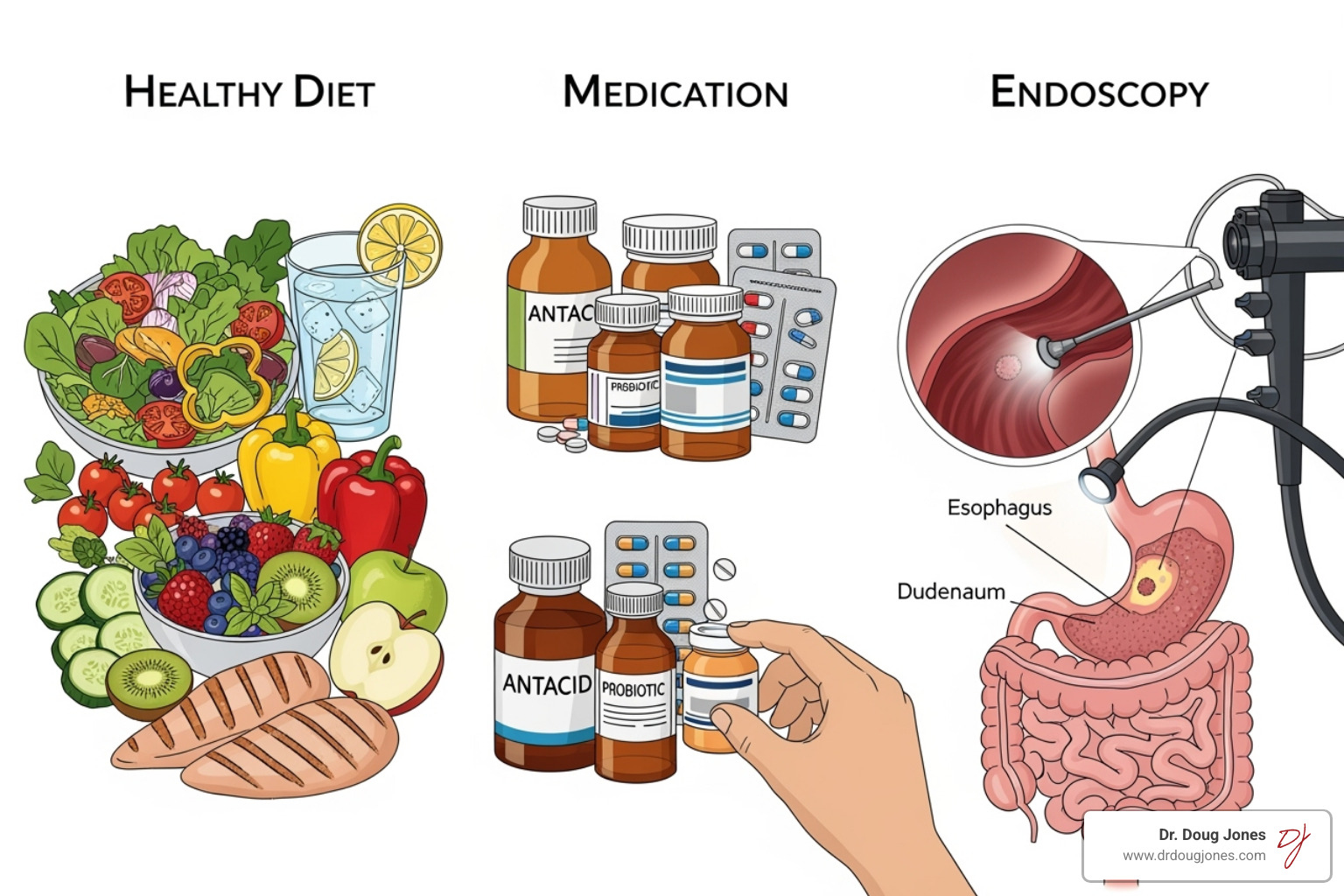
When facing an EoE diagnosis, it helps to know there's a proven roadmap. Eosinophilic esophagitis treatment centers on the "3 D's": Diet, Drugs, and Dilation. These are three powerful tools that can be used alone or in combination for maximum effect.
EoE treatment has two goals: making you feel better and achieving histologic remission—calming the inflammation at a cellular level. Achieving both gives you the best chance of preventing long-term complications like scarring. Modern EoE care is built on shared decision-making. Your lifestyle, preferences, and response to therapy all shape your personalized plan. There is no one-size-fits-all approach.
Understanding Your Diagnosis
An accurate diagnosis is the first step. This requires an upper endoscopy, the gold standard for viewing your esophagus. A gastroenterologist uses a thin, flexible tube with a camera to look for signs like rings, furrows, or white spots. The key part of the procedure is the biopsy—taking small tissue samples for analysis.
The diagnosis is confirmed when the lab finds ≥15 eosinophils per high-power field (eos/hpf) in your biopsy, combined with your symptoms. It's also important to differentiate EoE from GERD (acid reflux), as they can have similar symptoms but require different treatments. Having both a gastroenterologist and an allergist on your team is invaluable. The gastroenterologist manages the diagnosis and esophageal monitoring, while the allergist (like myself) helps identify triggers and manage related allergic conditions.
How Treatment Varies by Age and Severity
EoE presents differently depending on age, which changes our treatment approach. Personalized care is essential.
- Infants and toddlers often have feeding problems, refusing food or failing to gain weight. The goal is to restore normal pediatric growth.
- School-age children may complain of stomach aches, vomiting, or sudden picky eating. These feeding difficulties can be mistaken for a phase.
- Teenagers and adults primarily experience dysphagia—the feeling of food getting stuck. In severe cases, this can lead to a food impaction requiring emergency care.
A sobering fact drives home the need for early treatment: for every 10-year increase in age, the odds of developing a stricture (narrowing) doubles. This stricture risk highlights why consistent, long-term management is so important to prevent permanent damage to the esophagus.
Dietary Management: Identifying Your Food Triggers
The foods you eat every day could be triggering the inflammation in your esophagus. Unlike typical food allergies with immediate reactions, EoE triggers often cause delayed reactions, making it hard to connect your symptoms to specific foods. Standard skin prick or blood allergy tests are unreliable for identifying EoE triggers because EoE involves a different immune pathway.
This is where working with an experienced dietitian is invaluable. They can guide you through the process of identifying triggers without leaving you overwhelmed or nutritionally deficient. You can find helpful information and community through patient support resources like the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Once you identify your specific triggers, many people find dramatic relief.

Elimination Diets for Eosinophilic Esophagitis Treatment
The gold standard for identifying food triggers is an empiric elimination diet. This involves removing the most common trigger foods for 6 to 8 weeks, then reintroducing them one by one to see what causes a reaction.
The 6-food elimination diet (6-FED) removes milk, wheat, egg, soy, nuts, and fish. Research shows this approach achieves histologic remission in 68% of patients. While effective, it can be challenging. Less restrictive options include the 4-food elimination diet (dairy, wheat, egg, soy) or even a 2-food (dairy, wheat) or 1-food (dairy) approach.
After the elimination phase, a repeat endoscopy is needed to see if the inflammation has resolved. If it has, you'll begin the food reintroduction process, adding back one food group at a time, followed by another endoscopy to pinpoint the specific trigger. This process requires patience but provides a clear, personalized roadmap for your long-term eosinophilic esophagitis treatment.
Elemental Diets
An elemental diet is the most effective but also the most restrictive dietary treatment. It involves consuming only an amino acid-based formula containing pre-digested nutrients that your immune system doesn't recognize as threats. This gives your esophagus a complete break from inflammation.
However, the formulas can be unpalatable, and sticking to an all-liquid diet is difficult. Due to these adherence challenges, we typically reserve elemental diets for severe cases, for short-term use to achieve rapid remission, or as nutritional supplementation for children with growth issues.
Medical Therapies: A Guide to EoE Medications
When dietary changes aren't enough, medications are the next line of defense in eosinophilic esophagitis treatment. These therapies act as an inflammation-fighting toolkit, calming the immune response in your esophagus. The right medication depends on your symptom severity, lifestyle, and how your body responds. Your treatment plan should always be a collaboration with your healthcare provider.
Proton Pump Inhibitors (PPIs)
Surprisingly, common heartburn medications are often the first step in EoE treatment. Proton pump inhibitors (PPIs) not only reduce stomach acid but also have direct anti-inflammatory effects on the esophagus. A 2020 study found that twice-daily PPIs helped 41.7% of patients achieve histologic remission. They are generally well-tolerated and can provide quick symptom relief, especially if your symptoms overlap with acid reflux.
Topical Corticosteroids for Eosinophilic Esophagitis Treatment
Swallowed topical corticosteroids deliver medication directly to your esophageal lining. Unlike systemic steroids, they have minimal effects on the rest of your body. The two main options are budesonide (available as an oral suspension or dissolving tablet) and fluticasone (delivered via an inhaler, which you spray into your mouth and swallow).
These medications are highly effective. One study showed 58% of patients taking budesonide tablets had significant improvement in just 6 weeks. The main side effect is a risk of oral thrush (a yeast infection), which is easily prevented by rinsing your mouth with water after each dose and avoiding food or drink for 30 minutes.
Biologics and Advanced Treatments
For moderate-to-severe EoE that hasn't responded to other therapies, biologic therapies are a major breakthrough. These advanced medications target the specific immune pathways that drive EoE inflammation.
Dupilumab (Dupixent) is an FDA-approved weekly injection for patients 12 and older. It blocks IL-4 and IL-13, two key inflammatory proteins. By targeting the root cause with such precision, biologics can offer sustained relief with fewer side effects for patients with difficult-to-treat EoE. The field is advancing rapidly, and you can explore new and upcoming options on databases for information on advanced EoE treatments. This is an exciting time for EoE management, with new therapies offering hope to many.
Esophageal Dilation and Long-Term Outlook
While diet and medication address inflammation, eosinophilic esophagitis treatment sometimes requires addressing structural changes. Chronic inflammation can cause fibrosis (scar tissue), leading to a narrowing of the esophagus known as a stricture. Strictures make swallowing difficult and increase the risk of food getting stuck.
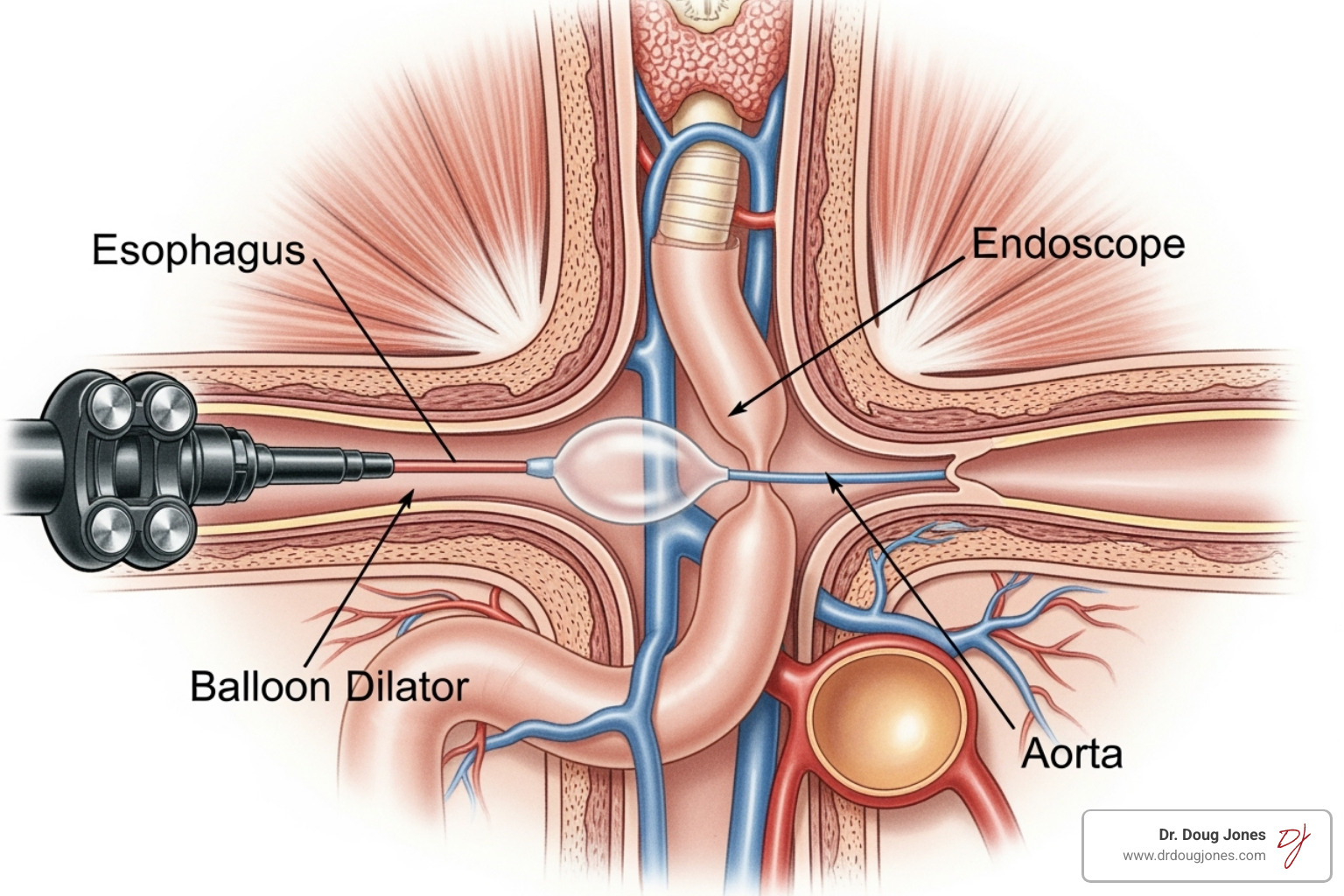
Esophageal dilation is a procedure where a gastroenterologist gently stretches these narrowed areas, restoring the normal opening so food can pass comfortably.
When is Esophageal Dilation Necessary?
Dilation is necessary when severe narrowing causes persistent swallowing problems or recurring food impactions. The procedure provides significant dysphagia relief and improves quality of life. However, it's crucial to understand that dilation is a mechanical fix; it does not treat the underlying inflammation. For this reason, dilation is almost always combined with anti-inflammatory therapy (diet or medication) to prevent the stricture from returning.
Preventing Complications and Managing EoE for Life
EoE is a chronic disease requiring lifelong management. The good news is that it's highly manageable with consistent treatment. Regular follow-up with your healthcare team is essential, even when you feel well, as symptoms don't always correlate with inflammation.
Monitoring with endoscopy at regular intervals helps catch issues early. The importance of maintenance therapy—whether diet or medication—cannot be overstated. Sticking to your treatment plan is the key to preventing relapses and avoiding long-term complications like irreversible fibrosis. A multidisciplinary team approach involving a gastroenterologist, allergist/immunologist, and dietitian is the most effective way to achieve long-term remission.
Frequently Asked Questions about EoE Treatment
It's natural to have questions about eosinophilic esophagitis treatment. Here are answers to some of the most common concerns I hear from patients.
How long does it take for EoE treatments to work?
The timeline for relief depends on the treatment. Symptom improvement can be quick, but confirming that the underlying inflammation is gone (histologic remission) takes longer and requires a follow-up endoscopy.
- Dietary Trials: 6-8 weeks to see histologic results.
- Proton Pump Inhibitors (PPIs): 4-12 weeks.
- Topical Corticosteroids: Can show improvement in as little as 6 weeks.
- Biologics: Clinical trials showed significant improvement by 24 weeks, with sustained results.
Feeling better doesn't always mean the inflammation is gone, so follow-up is key.
Can EoE be cured?
Currently, there is no cure for EoE. It is a chronic, lifelong condition. However, it is highly manageable. The goal of treatment is not a cure, but to achieve and maintain long-term remission. With consistent management, most patients lead full, healthy lives without symptoms or fear of food getting stuck. EoE becomes something you manage, rather than something that manages you.
What is the role of an allergist in my EoE treatment?
While a gastroenterologist diagnoses and monitors your esophagus, an allergist/immunologist like myself focuses on the immune system's role in EoE. Our contributions to your multidisciplinary care team include:
- Identifying Triggers: Guiding you through systematic dietary elimination to find your specific food triggers.
- Understanding environmental allergies: Often the focus is on food, but environmental allergies such as pollens and pets can also trigger and worsen EoE so these should be properly evaluated by an allergist.
- Managing Related Conditions: Many EoE patients also have asthma, eczema, or seasonal allergies. Treating these related atopic conditions can improve your EoE control.
- Guiding Therapy: We work with dietitians to ensure your diet is effective, safe, and nutritionally complete. We also help determine if environmental allergens play a role.
This collaborative team approach is the best way to create a personalized treatment plan that addresses all aspects of your health.
Take Control of Your EoE Journey
Living with Eosinophilic Esophagitis can be challenging, but empowerment through knowledge is your greatest ally. Understanding your options—diet, medication, and procedures—is the first step toward making informed decisions about your health.
There is no one-size-fits-all solution for EoE. Personalized treatment is key to achieving lasting relief. A multidisciplinary care team, including a gastroenterologist, dietitian, and an allergist/immunologist, is crucial for success. As a board-certified immunologist, Dr. Doug Jones's approach focuses on redefining complex immune challenges by digging deep to find the root causes of your EoE.
Your journey toward lasting relief doesn't have to be walked alone. We can work together to create a plan that fits your life and helps you reclaim the joy of eating without fear.
Ready to explore what personalized eosinophilic esophagitis treatment could look like for you?
Inquire about a personalized consultation




.png)